A variety of surgical tools and techniques can be used to perform a discectomy. An “open” technique uses a large skin incision and muscle retraction so that the surgeon can directly view the area. A “minimally invasive” technique, called a microendoscopic discectomy, uses a small skin incision. A series of progressively larger tubes, called dilators, are used to tunnel through the muscles. Special instruments help the surgeon see and operate in a smaller space. A minimally invasive incision causes less disruption of the back muscles and may decrease recovery time. Your surgeon will recommend the technique most appropriate for your specific case.
A fusion may be done at the same time as discectomy to help stabilize the spine for patients who are athletes, perform heavy labor, or have spinal instability. Fusion uses a combination of bone graft and hardware (screws/plates) to connect two vertebrae together. During the healing process, the two vertebrae fuse into one piece of bone. Fusion is rarely needed for a herniated lumbar disc [1].
Who is a candidate?
You may be a candidate for discectomy if you have:
- diagnostic tests (MRI, CT, myelogram) that show a herniated disc
- significant pain, weakness, or numbness in your leg or foot
- leg pain (sciatica) worse than back pain
- symptoms that have not improved with physical therapy or medication
- leg weakness, loss of feeling in the genital area, and loss of bladder or bowel control (cauda equina syndrome)
Posterior lumbar discectomy may be helpful in treating leg pain (sciatica) caused by:
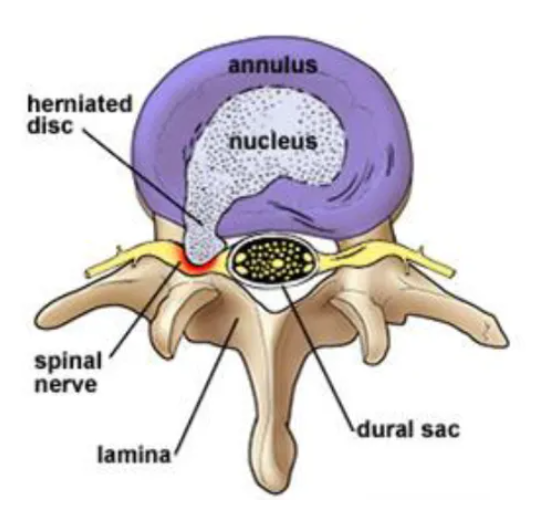
- Bulging or herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the surrounding wall (annulus). Irritation and swelling occurs when this material squeezes out and painfully presses on a nerve (Fig. 1).
- Degenerative disc disease: As discs naturally wear out, bone spurs form and the facet joints inflame. The discs dry out and shrink, losing their flexibility and cushioning properties. The disc spaces get smaller. These changes lead to stenosis or disc herniation.
The surgical decision
Most herniated discs heal after a few months of nonsurgical treatment. Your doctor may recommend treatment options, but only you can decide whether surgery is right for you. Be sure to consider all the risks and benefits before making your decision. Only 10% of people with herniated disc problems have enough pain after 6 weeks of nonsurgical treatment to consider surgery.
What happens before surgery?
You may be scheduled for presurgical tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. In the doctor’s office, you will sign consent and other forms so that the surgeon knows your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Discuss all medications (prescription, over-the-counter, and herbal supplements) you are taking with your health care provider. Some medications need to be continued or stopped the day of surgery.
Depending on your procedure you may be ask to lose weight in order to help in your recover results.
Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by the doctor. Additionally, stop smoking, chewing tobacco, and drinking alcohol 1 week before and 2 weeks after surgery because these activities can cause bleeding problems. No food or drink is permitted past midnight the night before surgery.
Morning of surgery
- Shower using antibacterial soap. Dress in freshly washed, loose-fitting clothing.
- Wear flat-heeled shoes with closed backs.
- If you have instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewelry at home (including wedding bands).
- Bring a list of medications (prescriptions, over-the-counter, and herbal supplements) with dosages and the times of day usually taken.
- Bring a list of allergies to medication or foods.
Arrive at the hospital 2 hours before (surgery center 1 hour before) your scheduled surgery time to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist will talk with you and explain the effects of anesthesia and its risks. An intravenous (IV) line will be placed in your arm.
What happens during surgery?
There are five steps of the procedure. The operation generally lasts 1 to 2 hours.
Step 1: prepare the patient
You will lie on your back on the operative table and be given anesthesia. Once asleep, you are rolled onto your stomach with your chest and sides supported by pillows. The area where the incision will be made is cleansed and prepped.
Step 2: make an incision
With the aid of a fluoroscope (a special X-ray), the surgeon passes a thin needle through the skin down to the bone to locate the affected vertebra and disc.
In an open discectomy, a skin incision is made down the middle of your back over the affected vertebrae (Fig. 2). The length of the incision depends on how many discectomies will be performed. A single-level incision is about 1 to 2 inches long. The back muscles are retracted on one side to expose the bony vertebra. An X-ray is taken to verify the correct vertebra.
In a minimally invasive discectomy, a small incision (less than 1 inch) is made to one side of your back (Fig. 3). Next, a series of progressively larger dilators are passed, one around the other, to gradually separate the muscles and create a tunnel to the bony vertebra.
Step 3: Make a laminotomy
Next, a small opening of the lamina, above and below the spinal nerve, is made with a drill or bone-biting tools (Fig. 4). A laminotomy can be done on one (unilateral) or both (bilateral) sides, or on multiple vertebrae levels.
Step 4: Remove the disc fragments
With the lamina removed, the surgeon gently retracts the protective sac of the nerve root. The surgeon looks through a surgical microscope to find the herniated disc. Only the ruptured portion of the disc is removed to decompress the spinal nerve root. The entire disc is not removed (Fig. 5). Bone spurs or a synovial cyst that may press on the nerve root are also removed.
Step 5: close the incision
The retractor holding the muscles is removed. The muscle and skin incisions are sewn together with sutures or staples. Steri-Strips are placed across the incision.
What happens after surgery?
You will awaken in the postoperative recovery area, called the PACU. Blood pressure, heart rate, and respiration will be monitored. Any pain will be addressed. Once awake, you will be moved to a regular room where you’ll increase your activity level (sitting in a chair, walking). Most patients can go home the same day. Other patients can be released from the hospital in 1 to 2 days.
Discharge instructions
Discomfort
After surgery, pain is managed with narcotic medication. Because narcotic pain pills are addictive, they are used for a limited period (2 to 4 weeks). As their regular use can cause constipation, drink lots of water and eat high fiber foods. Laxatives (e.g., Dulcolax, Senokot, Milk of Magnesia) can be bought without a prescription. Thereafter, pain is managed with acetaminophen (e.g., Tylenol).
Restrictions
If you had a fusion, do not use non-steroidal anti-inflammatory drugs (NSAIDs) (e.g., aspirin; ibuprofen, Advil, Motrin, Nuprin; naproxen sodium, Aleve) for 6 months after surgery. NSAIDs may cause bleeding and interfere with bone healing.
Do not drive for 2 to 4 weeks after surgery or until discussed with your surgeon.
Avoid sitting for long periods of time.
Do not lift anything heavier than 10 pounds (e.g., gallon of milk). Do not bend or twist at the waist. Housework and yard-work are not permitted until the first follow-up office visit. This includes gardening, mowing, vacuuming, ironing, and loading/unloading the dishwasher, washer, or dryer.
Postpone sexual activity until your follow-up appointment unless your surgeon specifies otherwise.
Do not smoke. Smoking delays healing by increasing the risk of complications (e.g., infection) and inhibits the bones' ability to fuse.
Activity
You may need help with daily activities (e.g., dressing, bathing) for the first few days. Fatigue is common. Let pain be your guide.
Gradually return to your normal activities. Walking is encouraged; start with a short distance and gradually increase to 1 to 2 miles daily. A physical therapy program may be recommended.
Bathing/Incision Care
You may shower 1 to 4 days after surgery. Follow your surgeon’s specific instructions. No tub baths, hot tubs, or swimming pools until your health care provider says it’s safe to do so.
Staples or stitches, which remain in place when you go home, will need to be removed. Ask your surgeon or call the office to find out when.
When To Call Your Doctor
If your temperature exceeds 101° F, or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
Recovery and Prevention
Schedule a follow-up appointment with your surgeon for 2 weeks after surgery. Physical therapy may be necessary for some people.
The recovery time varies from 1 to 4 weeks depending on the underlying disease treated and your general health. You may feel pain at the site of the incision. The original pain may not be completely relieved immediately after surgery. Aim to keep a positive attitude and diligently perform your physical therapy exercises if prescribed.
Most people can return to work in 2 to 4 weeks or less with jobs that are not physically challenging. Others may need to wait at least 8 to 12 weeks to return to work for jobs that require heavy lifting or operating heavy machinery.
Recurrences of back pain are common. The key to avoiding recurrence is prevention:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- A positive attitude and relaxation techniques (e.g., stress management)
- No smoking
What are the results?
Good results are achieved in 80 to 90% of patients treated with lumbar discectomy [2,3]. In a study that compared surgery and nonsurgical treatment for herniated discs, the outcomes were [2]: People with leg pain (sciatica) benefit more from surgery than those with back pain. People with less severe or improving pain do well with nonsurgical treatment. People with moderate to severe pain who had surgery notice a greater improvement than those who did not have surgery.
Similarly, minimally invasive discectomy techniques have been shown to be comparable in outcomes with open discectomy [4]. While the benefits of minimally invasive approaches include shorter operative time, less blood loss and muscle trauma, and faster recovery, these newer techniques are not appropriate for all patients. Ask your surgeon if minimally invasive microendoscopic discectomy is appropriate for you.
Discectomy may provide faster pain relief than nonsurgical treatment. However, it is unclear whether surgery makes a difference in what treatment may be needed later on. About 5 to 15% of patients will have a recurrent disc herniation, either at the same side or the opposite side.
What are the risks?
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. If spinal fusion is done at the same time as a discectomy, there is a greater risk of complications. Specific complications related to a discectomy may include:
Deep vein thrombosis (DVT) is a potentially serious condition caused when blood clots form inside the leg veins. If the clots break free and travel to the lungs, lung collapse or even death is a risk. However, there are several ways to treat or prevent DVT. Get up and out of bed as soon as possible so your blood is moving and less likely to clot. Support hose and pulsatile stockings can keep the blood from pooling in the veins. Drugs, such as aspirin, Heparin, or Coumadin, may also be used.
Lung problems. Lungs need to be working their best after surgery to provide tissues with enough oxygen to heal. If the lungs have collapsed areas, mucus and bacteria build up can lead to pneumonia. Your nurse will encourage you to breath deeply and cough often.
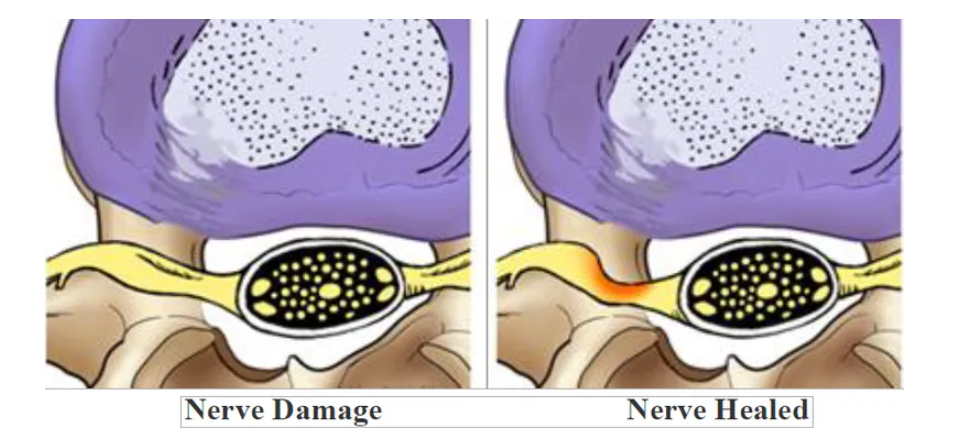
Nerve damage or persistent pain. Any operation on the spine comes with the risk of damaging the nerves or spinal cord. Damage can cause numbness or even paralysis. However, the most common cause of persistent pain is nerve damage from the disc herniation itself. Some disc herniations may permanently damage a nerve making it unresponsive to decompressive surgery (Fig. 6). In these cases, spinal cord stimulation or other treatments may provide relief. Be sure to go into surgery with realistic expectations about your pain. Discuss your expectations with your doctor.