Anterior Cervical Discectomy and Fusion
Anterior cervical discectomy and fusion (ACDF) is a surgery to remove a herniated or degenerative disc in the neck. An incision is made in the throat area to reach the front of the spine. The disc is removed and a graft is inserted to fuse together the bones above and below the disc. ACDF surgery may be recommend if physical therapy or medications fail to relieve your neck or arm pain caused by pinched spinal nerves. Patients typically go home the same day; recovery time takes 4 weeks.
What is an anterior cervical discectomy & fusion (ACDF)?
Discectomy literally means "cutting out the disc." A discectomy can be performed anywhere along the spine from the neck (cervical) to the low back (lumbar). The surgeon reaches the damaged disc from the front (anterior) of the spine through the throat area. By moving aside the neck muscles, trachea, and esophagus, the disc and bony vertebrae are exposed. Surgery from the front of the neck is more accessible than from the back (posterior) because the disc can be reached without disturbing the spinal cord, spinal nerves, and the strong neck muscles. Depending on your particular symptoms, one disc (single-level) or more (multi-level) may be removed.
After the disc is removed, the space between the bony vertebrae is empty. To prevent the vertebrae from collapsing and rubbing together, a spacer bone graft is inserted to fill the open disc space. The graft serves as a bridge between the two vertebrae to create a spinal fusion. The bone graft and vertebrae are fixed in place with metal plates and screws. Following surgery the body begins its natural healing process and new bone cells grow around the graft. After 3 to 6 months, the bone graft should join the two vertebrae and form one solid piece of bone. The instrumentation and fusion work together, similar to reinforced concrete.
Bone grafts come from many sources. Each type has advantages and disadvantages.
Autograft bone comes from you. The surgeon takes your own bone cells from the hip (iliac crest). This graft has a higher rate of fusion because it has bone-growing cells and proteins. The disadvantage is the pain in your hipbone after surgery. Harvesting a bone graft from your hip is done at the same time as the spine surgery. The harvested bone is about a half inch thick – the entire thickness of bone is not removed, just the top half layer.
Allograft bone comes from a donor (cadaver). Bone-bank bone is collected from people who have agreed to donate their organs after they die. This graft does not have bone-growing cells or proteins, yet it is readily available and eliminates the need to harvest bone from your hip. Allograft is shaped like a doughnut and the center is packed with shavings of living bone tissue taken from your spine during surgery.
Bone graft substitute comes from man-made plastic, ceramic, or bioresorbable compounds. Often called cages, this graft material is packed with shavings of living bone tissue taken from your spine during surgery.
After fusion you may notice some range of motion loss, but this varies according to neck mobility before surgery and the number of levels fused. If only one level is fused, you may have similar or even better range of motion than before surgery. If more than two levels are fused, you may notice limits in turning your head and looking up and down. Motion-preserving artificial disc replacements have emerged as an alternative to fusion. Similar to knee replacement, the artificial disc is inserted into the damaged joint space and preserves motion, whereas fusion eliminates motion. Outcomes for artificial disc compared to ACDF are similar, but long-term results of motion preservation and adjacent level disease are not yet proven. Talk with your surgeon about whether ACDF or artificial disc replacement is most appropriate for you.
Who is a candidate?
You may be a candidate for discectomy if you have:
- diagnostic tests (MRI, CT, myelogram) show that you have a herniated or degenerative disc
- significant weakness in your hand or arm
- arm pain worse than neck pain
- symptoms that have not improved with physical therapy or medication
ACDF may be helpful in treating the following conditions:
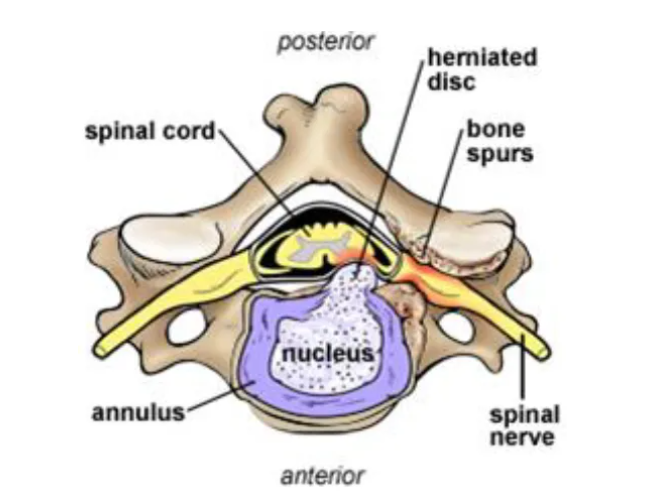
Bulging and herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the surrounding wall (annulus). Irritation and swelling occurs when this material squeezes out and painfully presses on a nerve.
Degenerative disc disease: As discs naturally wear out, bone spurs form and the facet joints inflame. The discs dry out and shrink, losing their flexibility and cushioning properties. The disc spaces get smaller. These changes lead to canal stenosis or disc herniation (Fig. 1).
The surgical decision
Most herniated discs heal after a few months of nonsurgical treatment. Your doctor may recommend treatment options, but only you can decide whether surgery is right for you. Be sure to consider all the risks and benefits before making your decision. Only 10% of people with herniated disc problems have enough pain after 6 weeks of conservative treatment to consider surgery.
Your surgeon will also discuss the risks and benefits of different types of bone graft material. Autograft is the gold standard for rapid healing and fusion, but the hip incision can be painful and at times lead to complications. Allograft (bone-bank) is more commonly used and has proven to be as effective for routine 1 and 2 level fusions in non-smokers.
What happens before surgery?
You may be scheduled for pre-surgical tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. In the doctor’s office, you will sign consent and other forms so that the surgeon knows your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, and previous surgeries). Discuss all medications (prescription, over-the-counter, and herbal supplements) you are taking with your health care provider. Some medications need to be continued or stopped the day of surgery.
Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by the doctor. Additionally, stop smoking, chewing tobacco, and drinking alcohol 1 week before and 2 weeks after surgery because these activities can cause bleeding problems. No food or drink is permitted past midnight the night before surgery.
Smoking
The most important thing you can do to ensure the success of your spinal surgery is quit smoking. This includes cigarettes, cigars, pipes, chewing tobacco, and smokeless tobacco (snuff, dip). Nicotine prevents bone growth and puts you at higher risk for a failed fusion. Patients who smoked had failed fusions in up to 40% of cases, compared to only 8% among non-smokers [1]. Smoking also decreases your blood circulation, resulting in slower wound healing and an increased risk of infection. Talk with your doctor about ways to help you quit smoking: nicotine replacements, pills without nicotine (Wellbutrin, Chantix), and tobacco counseling programs.
Morning of surgery
- Shower using antibacterial soap. Dress in freshly washed, loose-fitting clothing.
- Wear flat-heeled shoes with closed backs.
- If you have instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewelry at home (including wedding bands).
- Bring a list of medications (prescriptions, over-the-counter, and herbal supplements) with dosages and the times of day usually taken.
- Bring a list of allergies to medication or foods.
- Arrive at the hospital 2 hours before (surgery center 1 hour before) your scheduled surgery time to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist will talk with you and explain the effects of anesthesia and its risks. An intravenous (IV) line will be placed in your arm.
What happens during surgery?
There are seven steps to the procedure. The operation generally takes 1 to 3 hours.
Step 1: prepare the patient
You will lie on your back on the operative table and be given anesthesia. Once asleep, your neck area is cleansed and prepped. If a fusion is planned and your own bone will be used, the hip area is also prepped to obtain a bone graft. If a donor bone will be used, the hip incision is unnecessary.
Step 2: make an incision
An approximately 2-inch skin incision is made on the right or left side of your neck (Fig. 2). The surgeon makes a tunnel to the spine by moving aside muscles in your neck and retracting the trachea, esophagus, and arteries. Finally, the muscles that support the front of the spine are lifted and held aside so the surgeon can clearly see the bony vertebrae and discs.
Step 3: locate the damaged disc
With the aid of a fluoroscope (a special X-ray), the surgeon passes a thin needle into the disc to locate the affected vertebra and disc. The vertebrae bones above and below the damaged disc are spread apart with a special retractor.
Step 4: remove the disc
The outer wall of the disc is cut (Fig. 3). The surgeon removes about 2/3 of your disc using small grasping tools, and then looks through a surgical microscope to remove the rest of the disc. The ligament that runs behind the vertebrae is removed to reach the spinal canal. Any disc material pressing on the spinal nerves is removed.
Step 5: decompress the nerve
Bone spurs that press on your nerve root are removed. The foramen, through which the spinal nerve exits, is enlarged with a drill (Fig. 4). This procedure, called a foraminotomy, gives your nerves more room to exit the spinal canal.
Step 6. prepare a bone graft fusion
Using a drill, the open disc space is prepared on the top and bottom by removing the outer cortical layer of bone to expose the blood-rich cancellous bone inside. This “bed” will hold the bone graft material that you and your surgeon selected:
Bone graft from your hip. A skin and muscle incision is made over the crest of your hipbone. Next, a chisel is used to cut through the hard outer layer (cortical bone) to the inner layer (cancellous bone). The inner layer contains the bone-growing cells and proteins. The bone graft is then shaped and placed into the “bed” between the vertebrae (Fig. 5).
Bone bank or fusion cage. A cadaver bone graft or bioplastic cage is filled with the leftover bone shavings containing bone-growing cells and proteins. The graft is then tapped into the shelf space.
Step 7. close the incision
The spreader retractors are removed. The muscle and skin incisions are sutured together. Steri-Strips or biologic glue is placed across the incision.
What happens after surgery?
You will awaken in the postoperative recovery area, called the PACU. Blood pressure, heart rate, and respiration will be monitored. Any pain will be addressed. Once awake, you will be moved to a regular room where you’ll increase your activity level (sitting in a chair, walking). Patients who have had bone graft taken from their hip may feel more discomfort in their hip than neck incision. Most patients having a 1 or 2 level ACDF are sent home the same day. However, if you have difficulty breathing or unstable blood pressure, you may need to stay overnight.
Discharge instructions
Discomfort
After surgery, pain is managed with narcotic medication. Because narcotic pain pills are addictive, they are used for a limited period (2 to 4 weeks). As their regular use can cause constipation, drink lot of water and eat high fiber foods. Laxatives (e.g., Dulcolax, Senokot, Milk of Magnesia) can be bought without a prescription. Thereafter, pain is managed with acetaminophen (e.g., Tylenol).
Hoarseness, sore throat, or difficulty swallowing may occur in some patients and should not be cause for alarm. These symptoms usually resolve in 1 to 4 weeks.
Restrictions
- If you had a fusion, do not use non-steroidal anti-inflammatory drugs (NSAIDs) (e.g., aspirin; ibuprofen, Advil, Motrin, Nuprin; naproxen sodium, Aleve) for 6 months after surgery. NSAIDs may cause bleeding and interfere with bone healing.
- Do not smoke. Smoking delays healing by increasing the risk of complications (e.g., infection) and inhibits the bones' ability to fuse.
- Do not drive for 2 to 4 weeks after surgery or until discussed with your surgeon.
- Avoid sitting for long periods of time.
- Avoid bending your head forward or backward.
- Do not lift anything heavier than 5 pounds (e.g., gallon of milk).
- Housework and yard-work are not permitted until the first follow-up office visit. This includes gardening, mowing, vacuuming, ironing, and loading/unloading the dishwasher, washer, or dryer.
- Postpone sexual activity until your follow-up appointment unless your surgeon specifies otherwise.
Activity
You may need help with daily activities (e.g., dressing, bathing), but most patients are able to care for themselves right away.
Gradually return to your normal activities. Walking is encouraged; start with a short distance and gradually increase to 1 to 2 miles daily. A physical therapy program may be recommended.
If applicable, know how to wear a cervical collar before leaving the hospital. Wear it when walking or riding in a car.
Bathing/Incision Care
You may shower 1 to 4 days after surgery. Follow your surgeon’s specific instructions. No tub baths, hot tubs, or swimming pools until your health care provider says it’s safe to do so.
If you have staples or stitches when you go home, they will need to be removed. Ask your surgeon or call the office to find out when.
When to Call Your Doctor
If your temperature exceeds 101° F, or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
If your swallowing problems interfere with your ability to breathe or drink water.
Recovery and prevention
Schedule a follow-up appointment with your surgeon for 2 weeks after surgery. Recovery time generally lasts 4 to 6 weeks. X-rays may be taken after several weeks to verify that fusion is occurring. The surgeon will decide when to release you back to work at your follow-up visit.
A cervical collar or brace is sometimes worn during recovery to provide support and limit motion while your neck heals or fuses (see Braces & Orthotics). Your doctor may prescribe neck stretches and exercises or physical therapy once your neck has healed.
If you had a bone graft taken from your hip, you may experience pain, soreness, and stiffness at the incision. Get up frequently (every 20 minutes) and move around or walk. Don’t sit or lie down for long periods of time.
Recurrences of neck pain are common. The key to avoiding recurrence is prevention:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- A positive attitude and relaxation techniques (e.g., stress management)
- No smoking
What are the results?
Anterior cervical discectomy is successful in relieving arm pain in 92 to 100% of patients [3]. However, arm weakness and numbness may persist for weeks to months. Neck pain is relieved in 73 to 83% of patients [3]. In general, people with arm pain benefit more from ACDF than those with neck pain. Aim to keep a positive attitude and diligently perform your physical therapy exercises.
Achieving a spinal fusion varies depending on the technique used and your general health (smoker). In a study that compared three techniques: ACD, ACDF, and ACDF with plates and screws, the outcomes were [3]:
67% of people who underwent ACD (no bone graft) achieved fusion naturally. However, ACD alone results in an abnormal forward curving of the spine (kyphosis) compared with the other techniques. 93% of people who underwent ACDF with bone graft placement achieved fusion. 100% of people who underwent ACDF with bone graft placement and plates and screws achieved fusion.
What are the risks?
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots (deep vein thrombosis), and reactions to anesthesia. If spinal fusion is done at the same time as a discectomy, there is a greater risk of complications. Specific complications related to ACDF may include:
Hoarseness and swallowing difficulties. In some cases, temporary hoarseness can occur. The recurrent laryngeal nerve, which controls the vocal cords, is affected during surgery. It may take several months for this nerve to recover. In rare cases (less than 1/250) hoarseness and swallowing problems may persist and need further treatment with an ear, nose and throat specialist.
Vertebrae failing to fuse. There are many reasons why bones do not fuse together. Common ones include smoking, osteoporosis, obesity, and malnutrition. Smoking is by far the greatest factor that can prevent fusion. Nicotine is a toxin that inhibits bone-growing cells. If you continue to smoke after your spinal surgery, you could undermine the fusion process.
Hardware fracture. Metal screws and plates used to stabilize the spine are called “hardware.” The hardware may move or break before the bones are completely fused. If this occurs, a second surgery may be needed to fix or replace the hardware.
Bone graft migration. In rare cases (1 to 2%), the bone graft can move from the correct position between the vertebrae soon after surgery. This is more likely to occur if hardware (plates and screws) is not used or if multiple vertebral levels are fused. If this occurs, a second surgery may be necessary.
Transitional syndrome. Fusion of a spine segment causes extra stress and load to be transferred to the discs and bones above or below the fusion. The added wear and tear can eventually degenerate the adjacent level and cause pain.
Nerve damage or persistent pain. Any spine surgery comes with the risk of damaging the nerves or spinal cord. Damage can cause numbness or even paralysis. However, the most common cause of persistent pain is nerve damage from the disc herniation itself. Some disc herniations may permanently damage a nerve making it unresponsive to surgery. Like furniture on the carpet, the compressed nerve doesn't spring back. In these cases, spinal cord stimulation or other treatments may provide relief.
If you have any questions please don’t hesitate to contact us 209-349-8429.
rEQUEST AN APPOINTMENT
Fill out to form to request an appointment. You can also ask us spine care related questions. We will get back to you ASAP.







